Originally Authored by Emily J. Helder, Emily Austria, Maureen Lacy, and David M. Frim in the Journal of Pediatric Neurology
Abstract
Neuropsychiatric disease is often prevalent in white matter disorders. Hydrocephalus, for example, causes a disruption of white matter pathways. While research has shown that emotional and behavioral problems are prevalent in myelomeningocele (MMC) associated hydrocephalus, it is less clear if this is true in hydrocephalus due to other etiologies. The present study compared 30 children with early onset communicating shunted hydrocephalus with 18 healthy controls (age range 6–16 years) with regard to parent rated behavior and emotional functioning, controlling for intelligence quotient differences between groups. Results indicated that children with communicating hydrocephalus have a higher incidence of clinically significant reported behavioral/emotional difficulties (30%) compared with controls (11%). Internalizing problems were significantly more common in patients compared to controls. These findings underscore the importance of monitoring behavioral and emotional adjustment in children with hydrocephalus and intervening as appropriate. In addition, these observations show that MMC children with hydrocephalus and congenital hydrocephalus patients have similar emotional difficulties implying that it is hydrocephalus and not other MMC-associated brain anomalies that affect emotional outcome.
Keywords: Congential hydrocephalus, internalization, emotional problems
Introduction
Neuropsychiatric conditions such as depression, anxiety, and apathy are often associated with white matter diseases. Multiple sclerosis, acute disseminated encephalomyelitis, neurosarcoidosis, systemic lupus erythematosus, and vascular dementia have a higher prevalence of psychiatric disorders than seen in the general population and other non-white matter diseases [1]. While a reactive state may be playing a role, there is a growing body of evidence that white matter pathology is directly associated with occurrence of these neuropsychiatric states [1].
Congenital hydrocephalus is a neurological condition resulting in excessive buildup of cerebral spinal fluid which disrupts white matter tract development and myelination [2,3]. Therefore, in theory, children with hydrocephalus are at increased risk for neuropsychiatric disorders. Research has in fact shown that children with myelomeningocele (MMC) associated hydrocephalus have been found to have higher rates of behavioral problems on standardized rating scales [4]. Connell and McConnel [5] found 44% of their heterogeneous sample of children with congenital shunted hydrocephalus met criteria for a psychiatric disorder based on parent ratings and interviews, while Donders et al. [6] found a rate of 16% based on the Personality Inventory for Children-Revised in a heterogeneous sample including 27% with MMC-associated hydrocephalus. Recently, Lindquist et al. [7] found that parents of a mixed group of children with MMC-associated hydrocephalus or infantile hydrocephalus reported that at least 75% their children suffered from at least one behavioral problem based on the Conner’s Rating Scale. While learning problems were seen in almost half, conduct problems (17%), hyperactivity (32%), inattentiveness (17%), psychosomatic issues (29%), and anxiety (12%) were also elevated compared to healthy peers. The authors noted that these rates are much higher than seen in epidemiological studies, where only 7% of children were labeled as having a psychiatric disorder and 3 to 5% with attention deficit disorder [8].
While it is apparent that the rates of behavioral problems are higher in MMC-associated hydrocephalus, it is less clear if this is true in patients with hydrocephalus associated with other etiologies. Swartwout et al. [9] found that children with aqueductal stenosis performed better on tests of attention compared to children with spina bifida suggesting that there may be different symptoms based on etiology. Given that, the majority of patients participating in these studies have MMC it is important to recognize that the MMC child has his/her own unique brain morphology that includes anatomical anomalies. While hydrocephalus may play a role in overall outcome, neural tube defects such as MMC directly impact brain development. The neuroembroyogenesis has been shown to adversely impact development of the corpus callosum, midbrain, and cerebellum [4], all structures that can play a role in neurobehavioral development [10]. Additionally, children with MMC also experience unique motor difficulties that may impact emotional status that are not encountered by children with hydrocephalus without spinal cord involvement.
While Fletcher et al. [11] found that group difference in etiology did not influence the presence of behavioral problems; the defined groups were heterogeneous and small. For example, nine of the 19 patients defined as “prematurity hydrocephalus group” were not shunted and there were only nine children in the aqueduct stenosis sample. While not finding any statistically significant influence of etiology on outcome, 44% of the children with aqueductal stenosis compared to 26% of children with MMC-associated hydrocephalus were viewed by their parents as displaying psychiatric symptoms, primarily internalizing behaviors.
In the Lindquist et al. [7] study, etiology was also unclear within the group described as “infantile hydrocephalus” simply defined as “not associated with MMC”. Hydrocephalus can be due to many causes (e.g., aqueductal stenosis, cysts, periventricular hemorrhage, and trauma) and subtle differences in etiology may impact functional outcome in these studies. In fact, Lindquist et al. [7] found that the children with infantile hydrocephalus tended to display more hyperactivity while those with MMC displayed more passive/inattentive behaviors.
Along with issues of etiology, the impact of intellect is sometimes considered and other times ignored in studies. Research has consistently shown that children with hydrocephalus display limitations in intellect [4, 12]. Furthermore, Lindquist et al. [7] found that intellect impacted endorsement of behavioral problems in children, with lower intellect related to greater endorsement of behavioral difficulties.
The purpose of this study was to further our understanding of the incidence and type of psychiatric dysfunction associated with hydrocephalus by examining a homogeneous group of children, without MMC, with early shunted hydrocephalus controlling for intellectual functioning. Based on prior research noting increased rates of depression, anxiety, attention, and apathy associated with white matter diseases [1], it was hypothesized that children with early shunted communicating hydrocephalus in the absence of other disease (e.g., MMC) will demonstrate higher rates of these psychiatric disorders than seen in peers or general popultion. Alternatively, the null hypothesis for the current study would be that children with hydrocephalus would have statistically equivalent rates of parent rated behavior and emotional difficulties in comparison to healthy, same age peers.
Materials and methods
After Institutional Review Board approval, participants were recruited through the Pediatric Neurosurgery Service at The University of Chicago. All participants provided their assent and their legal guardians provided informed consent following a full explanation of the study procedures. The participants included 30 children with hydrocephalusand 18 healthy children without hydrocephalus that served as a control group. The control group consisted of typically developing, healthy siblings and friends of the children in the patient group. The control group contained 12 males and six females and had a mean age of 135 – 34 months (range 76–190 months). The hydrocephalus group had a mean age of 116 43 months (range 73–192 months) and was composed of 20 males and 10 females. All subjects within the hydrocephalus group presented with communicating (absorptive) hydrocephalus from either documented or presumed pre- or perinatal intraventricular hemorrhage. Other causes of absorptive hydrocephalus (i.e., meningitis) or anatomic anomalies associated with absorptive hydrocephalus (i.e., Dandy- Walker cyst) were excluded. All children with hydrocephalus were shunted in the first year of life with a non-siphoning valve shunt system that was placed in a ventriculoperitoneal position. For preterm infants requiring shunting, shunts were not placed until children attained a weight of 1750 g or greater with lumbar puncture used to control hydrocephalus until that time. External drainage devices were not used in the cohort presented in this study. Children born at term requiring shunting were shunted immediately. Children who developed hydrocephalus within their first year requiring shunting were also shunted immediately. Patients were excluded if they had a history of shunt infection or revision in the year prior to study participation. Six participants had a history of distant shunt infection and each of those six had more than three shunt revisions (21%).
Additionally, children with full scale intelligence quotient (FSIQ) (as measured by the Wechsler Intelligence Scale for Children-Third Edition) scores less than 70 were also excluded due to concerns that the behavioral and emotional rating scale would be less valid in children with intellectual disability. Of the participants with hydrocephalus, 11 (36.7%) were born pre- mature, six (20%) who were born at term had visible pre-or post-natal brain hemorrhage, and five (16.7%) had a history of having a seizure without ongoing epilepsy.
Behavioral and emotional adjustment was assessed using the Parent Rating Scale of the Behavior Assessment Scales for Children (BASC, 13). The BASC assesses the presence and severity of a range of behavioral and emotional difficulties by comparing responses of an individual parent about their child to a large, age-matched, normative sample. A total of nine clinical scales are included: Hyperactivity, Aggression, Conduct Problems, Anxiety, Depression, Somatization, Atypicality, Withdrawal, and Attention Problems. Social skills and leadership qualities are also rated as an assessment of adaptive functioning. Composite scores can be derived for externalizing and internalizing problems as well as adaptive skills and an overall Behavioral Symptom Index. Scores on all scales and composites are interval level data and have a mean of 50 and a standard deviation of 10. Higher scores on the clinical scales, internalizing and externalizing composite scores, and behavioral symptoms index indicate worse behavioral functioning. In contrast, higher scores on the adaptive scales and adaptive composite indicate better adaptive functioning. Conventional cut-off scores [13] were used, with a T-score of 60– 69 indicating difficulties in the “at-risk” range and T- scores of greater than or equal to 70 indicative of “clinically significant” difficulties for the clinical scales and composite scores. For the adaptive scales and adaptive composite, “at-risk” corresponded to T-scores of 31–40 while “clinically significant” corresponded to T-scores of less than or equal to 30.
Participants also received a comprehensive assessment battery at the same visit as parents completed the Parent Rating Scale of the BASC, including assessment of intelligence (Wechsler Intelligence Scale for Children-Third Edition, WISC-III), which was later used as a covariate in selected analyses. The data derived from parent ratings was normally distributed, with no significant skew or kurtosis, thus, independent samples t-tests were used to compare the hydrocephalus and control groups in age and FSIQ, while a Chi-square test was used to evaluate possible differences between groups on gender distribution. In order to assess for differences between groups on behavioral and emotional adjustment, independent samples t-tests were used to compare groups across the clinical scales and composites. ANCOVA’s were also used to examine differences between groups on behavioral ratings while using FSIQ as a covariate. Additionally, the incidence of clinical scales falling in the “at risk” and “clinically significant” range were compared between groups using a Chi-square test.
Results
The participants with hydrocephalus and the control group did not differ with regard to gender distribution or age at the time of study. The groups did, however, differ with regard to FSIQ (t [46] = 4.1, P < 0.01). Though both groups were within the broad average range of intelligence, the hydrocephalus group had a significantly lower FSIQ (91 plus or minus 11) compared with the control group (108 plus or minus 18).
Participants with hydrocephalus were compared to controls across the nine clinical scales, two adaptive behavior scales, and four composite scores on the BASC.
Results revealed significant differences (P < 0.05) across several clinical scales and composites, with hydrocephalic patients rated as having significantly more difficulty than controls (Table 1).
With regard to the BASC clinical scales, participants with hydrocephalus had worse parent-rated depression (t [46] = 1.98, P < 0.05), somatization (t [46] = 2.45, P < 0.05), atypicality (t [46] = 2.41, P < 0.05), and attention problems (t [46] = 2.22, P < 0.05). Additionally, the internalizing composite score (t [46] = 2.38, P < 0.05) and overall behavioral symptoms index (t [46] = 2.24, P < 0.05) were also significantly higher in children with hydrocephalus compared to controls. No differences were observed between groups across adaptive scales (Social Skills t [46] = 0.295, P = 769; Leadership t [46] = 1.22, P = 228) or the adaptive composite (t [46] = 657, P = 514).
Given the significant difference between groups on the FSIQ measure, univariate ANCOVA’s, controlling for FSIQ, were used to compare groups across clinical, adaptive, and composite scores. FSIQ was not a significant predictor across these analyses with the exception of the depression clinical scale. Inclusion of FSIQ as a covariate in that analysis resulted in increasing the magnitude of the significant difference between hydrocephalus participants and controls (F [2, 48] = 7.605, P < 0.01).
Additionally, the incidence of “at-risk” and “clinically significant” behavior and emotional difficulties were calculated for both groups (Table 2). Despite the fact that “at-risk” scores fall below the standard clinical cut-off for the BASC, the decision was made to include them in order to provide a more dimensional view of behavioral and emotional adjustment in this sample as well as because it provides an opportunity to compare the current results with other studies that have used a lower cut-off (i.e., T = 65, 10). Within the control group, a minority (11%) of children were found to have “clinically significant” elevations on at least one of the scales and composites. “Clinically significant” elevations on at least one scale were observed in 30% of the hydrocephalus group. Also, “at-risk” range difficulties with attention and withdrawal as well as “clinically significant” conduct problems were more likely in the hydrocephalus group compared with controls. Adaptive skills were rated quite similarly between controls and children with hydrocephalus.
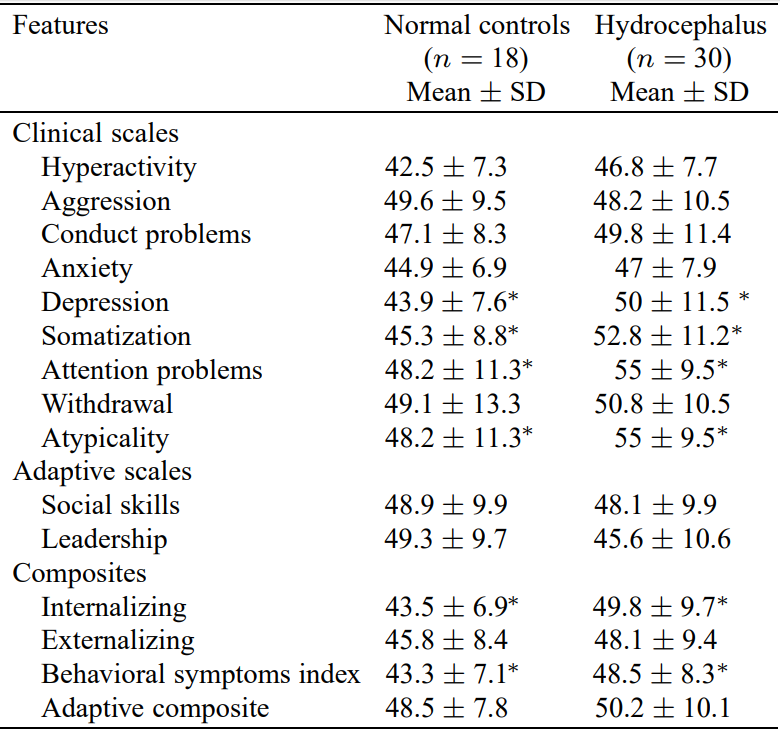
∗P < 0.05.
Discussion

Incidence of behavioral and emotional difficulties across groups
The current study sought to examine the incidence and pattern of behavioral and emotional difficulties in a homogeneous sample of children with early shunted hydrocephalus when compared with a control group of healthy, typically developing children who were statistically equivalent with regard to age at time of testing and gender distribution. None of the patients were diagnosed with MMC. Based on prior research indicating intelligence may be compromised in this population [12] and may impact ratings of emotional problems [7], intelligence was used as a covariate in appropriate analyses.
Results revealed an increased incidence of clinically significant behavioral and emotional difficulties in children with non-MMC-associated hydrocephalus when compared to the control group (30% vs. 11%). Examination of the significant differences between patients and controls revealed that children with early shunted congenital hydrocephalus had higher parent ratings on several scales including depression, somatization, atypicality, and attention problems. Unlike the study of Lindquist et al. [7] finding of a trend toward increased hyperactivity in her sample of “infantile” hydrocephalus (38%) compared to MMC-associated hydrocephalus (23%), none of our patients with early shunted communicating hydrocephalus were reported by parents as hyperactive. While there was a significant finding between our groups on atypicality which may suggest autism spectrum symptoms, this was driven by one patient in the at-risk category (3%) compared to Lindquist et al. [7] finding of 20%. Linquist’s group was defined as a “hydrocephalus with a wider spectrum of underlying pre, peri, or early postnatally acquired brain lesions” and thus this may account for the finding of more severe behavioral problems in that sample. Additionally, Lindquist et al. [7] use of a lower cut-off to determine “clinically significant” difficulties (T > 65 versus T > 70) may have also contributed to the differences between their findings and the current study.
Consistent with the trend of higher parent report of internalizing behaviors in certain groups [11], the current sample documented that parents reported a higher rate of internalizing behavior compared to age matched peers, even when controlling for intelligence. This pattern of findings is consistent with previous research. Internalizing problems, such as depression, are more commonly seen in white matter diseases [14] and now across etiologies of hydrocephalus. Finally, attention problems were found in the current study and have been commonly reported both in studies using parent report [15] and in research that utilizes direct cognitive testing [16]. In the present study, the somatization scale may have been rated more highly in the hydrocephalus group due to the use of a healthy, typically developing control group, rather than children with other medical difficulties.
Overall, this finding is consistent with past research suggesting that individuals with hydrocephalus are at a higher risk of developing difficulties compared with healthy controls [17] as well as children with other medical difficulties [11]. Review of the patterns of incidence of “at risk” and “clinically significant” behavioral and emotional difficulties reported by the parents in the present study, though exploratory in nature, revealed a wide variability in the presentation of children with this form of hydrocephalus. Though internalizing difficulties such as withdrawal (i.e., “prefers to be alone”, “avoids other children”) were significantly more common in the hydrocephalus group compared with controls, a wide variety of both internalizing and externalizing problems were endorsed at clinically significant levels across the sample. This is consistent with Donders et al. [6] finding of wide variability in their sample as well. Of note, only two of the children in our hydrocephalus group had elevations on more than one of the clinical scales, thus underscoring the variability in presentation across this sample.
These findings may be related to several factors. In the present study, children in the patient group were compared with age comparable healthy peers. It is likely that some of the elevation in behavioral and emotional difficulties may be related to children with hydrocephalus being forced to cope with multiple factors, including the challenge of feeling or looking different than peers, the process of undergoing multiple medical procedures, and the limitations on involvement in age- typical activities. Population based research has suggested that these types of factors continue to influence adjustment into adulthood [18].
However, similar incidences and patterns of behavioral and emotional difficulties have been found even when comparing children with MMC-associated hydrocephalus to children with other chronic neurological difficulties [11]. Thus, biological changes specific to hydrocephalus may also underlie the increased incidence of emotional difficulties. Specifically, hydrocephalus significantly impacts white matter functioning and development [19,20]. Also, there is significant evidence in adults that white matter changes or subcortical injuries are related to the development of depression [21,22]. The finding in the present study that children with hydrocephalus are at a higher risk for displaying internalizing problems, may therefore be related to the disruption of white matter pathways during development. The attention problems reported in the present study and in the broader literature regardless of etiology of hydrocephalus may also be tied to alterations in fronto-subcortical circuits important for executive functioning. Future longitudinal imaging studies would be required to more carefully evaluate the impact of brain changes on behavior and emotional adjustment.
Several limitations are present in the current study. First, behavioral and emotional adjustment were measured solely based on parent report. Future research could also include self and teacher ratings in order to more comprehensively identify children with areas of difficulty. A second limitation is the relatively small sample size. Due to this factor, a number of interesting hypotheses were not possible to address statistically due to concerns about limited power. This included examining whether the presence of certain medical complications (i.e., seizures, shunt revisions) places individuals with hydrocephalus at greater risk for development of behavioral or emotional difficulties.
Taken as a whole, the results of the present study suggest that children with hydrocephalus are at an increased risk to develop difficulties with behavioral and emotional adjustment. Internalizing problems and attentional difficulties are the most commonly reported difficulties, though a wide variety of clinically significant externalizing and internalizing difficulties were also seen. Our results, when compared with other studies reporting consistent findings in mixed populations [7,11], suggest that the emotional/behavioral difficulties seen are related to the hydrocephalus and/or its treatment, rather than any associated anomalies (i.e., MMC). As such, the underlying anatomic substrate for these behavioral issues is more likely effects of the hydrocephalus (e.g., while matter stretch and injury) than the etiology of the hydrocephalus.
Future research, utilizing longitudinal designs, is necessary to further examine the development of these difficulties over time and to identify specific factors that may either protect individuals or increase the risk for development of behavior and emotional problems. Careful imaging studies of these populations will help elucidate the underlying anatomical anomalies that may accompany these behavioral changes.
References
- J.G. Harris and C.M. Filley, CADASIL: neuropsychological findings in three generations of an affected family, J Int Neuropsychol Soc 7 (2001), 768–774.
- M.R. Del Bigio, Neuropathological changes caused by hydrocephalus, Acta Neuropathol 85 (1993), 573–585.
- W. Yuan, F.T. Mangano, E.L. Air et al., Anisotropic diffusion properties in infants with hydrocephalus, a Diffusion Tensor Imaging Study AJNR Am J Neuroradiol 30 (2009) 1792–1798.
- K.O. Yeates, J.M. Fletcher and M. Dennis, Spina bifida and hydrocephalus, in: Handbook of Neuropsychology, J.E. Morgan and J.H. Ricker, eds, New York: Taylor & Francis, 2008, pp. 128–148.
- H.M. Connell and T.S. McConnel, Psychiatric sequelae in children treated operatively for hydrocephalus in infancy, Dev Med Child Neurol 23 (1981), 505–517.
- J. Donders, B.P. Rourke and A.I. Canady, Emotional adjustment of children with hydrocephalus and of their parents, J Child Neurol 7 (1992), 375–380.
- B. Lindquist, G. Carlsson, E.K. Persson and P. Uvebrant, Behavioural problems and autism in children with hydrocephalus: a population-based study, Eur Child Adolesc Psychiatry 15 (2006), 214–219.
- M. Rutter, J. Tizard, W. Yule, P. Graham and K. Whitmore, Research report: Isle of Wight Studies, 1964-1974, Psychol Med 6 (1976), 313–332.
- M.D. Swartwout, P.T. Cirino, A.W. Hampson, J.M. Fletcher, M.E. Brandt and M. Dennis, Sustained attention in children with two etiologies of early hydrocephalus, Neuropsychology 22 (2008), 765–775.
- B.K. Kleinschmidt-Demasters, A.M. Rojiani and C.M. Filley, Central and extrapontine myelinolysis: then… and now, J Neuropathol Exp Neurol 65 (2006), 1–11.
- J.M. Fletcher, B.L. Brookshire, S.H. Landry et al., Behavioral adjustment of children with hydrocephalus: relationships with etiology, neurological, and family status, J Pediatr Psychol 20 (1995), 109–125.
- M. Lacy, M. Oliveira, E. Austria and M.D. Frim, Neurocognitive outcome after endoscopic third ventriculocisterostomy in patients with obstructive hydrocephalus, J Int Neuropsychol Soc 15 (2009), 394–398.
- C.R. Reynolds and R.W. Kamphaus, The Behavior Assessment System for Children, American Guidance Service Inc (1999).
- C.M. Filley, The neuroanatomy of attention, Semin Speech Lang 23 (2002), 89–98.
- E.M. Mahone, T.A. Zabel, E. Levey, M. Verda and S. Kinsman, Parent and self-report ratings of executive function in adolescents with myelomeningocele and hydrocephalus, Child Neuropsychol 8 (2002), 258–270.
- P. Hellstro¨m, M. Edsbagge, T. Archer, M. Tisell, M. Tullberg and C. Wikkelsø, The neuropsychology of patients with clinically diagnosed idiopathic normal pressure hydrocephalus, Neurosurgery 61 (2007), 1219–1228.
- B.M. Rose and G.N. Holmbeck, Attention and executive functions in adolescents with spina bifida, J Pediatr Psychol 32 (2007), 983–994.
- N. Gupta, J. Park, C. Solomon, D.A. Kranz, M. Wrensch and Y.W. Wu, Long-term outcomes in patients with treated childhood hydrocephalus, J Neurosurg 106(Suppl 5) (2007), 334–339.
- M.R. Del Bigio, M.C. da Silva, J.M. Drake and U.I. Tuor, Acute and chronic cerebral white matter damage in neonatal hydrocephalus, Can J Neurol Sci 2 (1994), 299–305.
- M.R. Del Bigio, M.J. Wilson and T. Enno, Chronic hydrocephalus in rats and humans: white matter loss and behavior changes, Ann Neurol 53 (2003), 337–346.
- G.S. Figiel, K.R. Krishnan, P.M. Doraiswamy, V.P. Rao, C.B. Nemeroff and O.B. Boyko, Subcortical hyperintensities on brain magnetic resonance imaging: a comparison between late age onset and early onset elderly depressed subjects, Neurobiol Aging 12 (1991), 245–247.
- R. Bakshi, D. Czarnecki, Z.A. Shaikh et al., Brain MRI lesions and atrophy are related to depression in multiple sclerosis, Neuroreport 11 (2000), 1153–1158.
